TL;DR:
- Direct Primary Care (DPC) involves a monthly fee directly paid to providers, covering most primary care services without insurance hassle.
- Telemedicine allows digital healthcare consultations via video calls or messaging.
- Benefits of DPC + Telemedicine:
- Remote consultations enhance convenience.
- Cost reduction by eliminating insurance middlemen.
- Improved chronic disease management through frequent check-ins.
- Challenges include technology access, regulatory compliance, and reimbursement issues.
- Technology requirements: Video conferencing, secure platforms, and reliable internet are essential.
- Success stories highlight increased patient satisfaction and better health outcomes, especially in underserved areas like rural communities.
Do you ever feel stuck waiting days to get a simple check-up? Imagine video chatting with your doctor in your PJs without leaving home. That’s where telemedicine in Direct Primary Care (DPC) comes in. It’s like having a doctor on speed dial. In this post, we’ll geek out on how combining telemedicine with DPC isn’t just convenient but a game-changer for your healthcare. Ready to learn how you can get top-notch care from your couch? Let’s dive in!
Understanding Telemedicine in Direct Primary Care
Direct Primary Care (DPC) is a healthcare model where patients pay a monthly or annual fee directly to their primary care provider. This fee covers most primary care services, removing the need for traditional insurance billing. Say goodbye to insurance hassles! Patients get more personalized and direct access to their doctors.
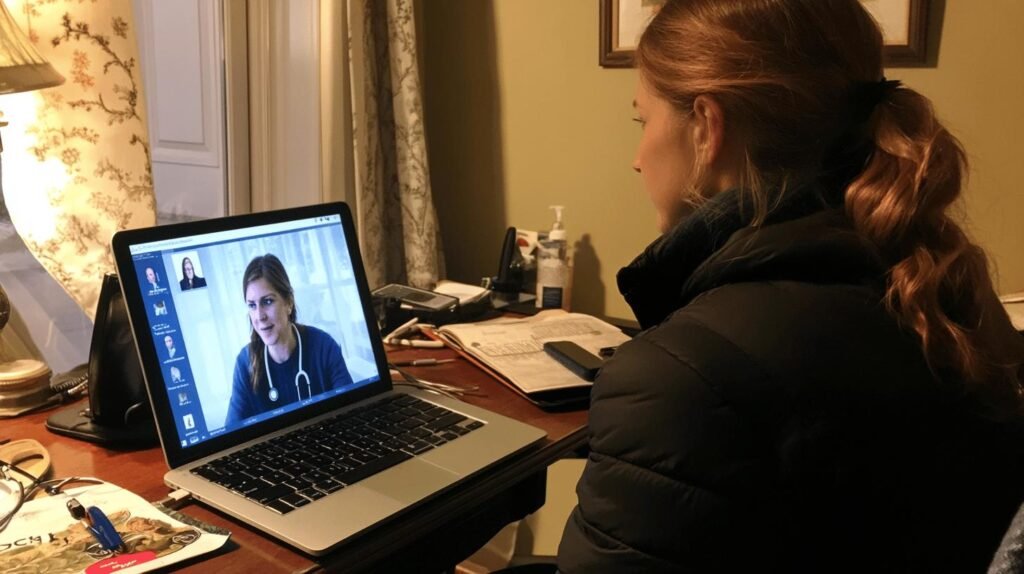
Telemedicine, also known as telehealth, lets patients receive healthcare services digitally. Think online consultations through your computer, tablet, or smartphone. It’s like having a doctor’s visit without leaving your couch! This digital approach allows for more flexible and convenient healthcare options, especially for those with busy schedules or mobility issues.
When you combine DPC with telemedicine, you create a virtual direct primary care model. Pretty cool, right? This combo means you can access your primary care provider through video conferences and secure messages. There is no need to drive to the clinic for every little concern. It enhances patient access, making healthcare more convenient and efficient. Whether managing chronic conditions or getting a quick consultation, this integration elevates the quality of care.
The impact of this integration on patient care is enormous. Patients enjoy more timely and accessible healthcare, which can lead to better health outcomes. Regular and accessible communication with your doctor means you can address health issues before they escalate. Plus, the convenience of telemedicine means fewer missed appointments and more proactive healthcare management. It’s a win-win for both patients and providers!
Benefits of Telemedicine in Direct Primary Care

Regarding Direct Primary Care (DPC), telemedicine is like adding a turbo boost to an already excellent model. One of the most incredible perks? Increased access and convenience. Imagine not having to drive to the clinic for every little thing. Telemedicine allows you to consult with your doctor from the comfort of your home. This is especially handy for folks dealing with chronic conditions, mental health issues, or just a super busy schedule. You can get the care you need without all the hassle.
Another big win here is reduced healthcare costs. Since you’re cutting out the middlemen (those pesky insurance companies), you and your doctor save money. Telemedicine also helps manage chronic diseases more effectively. You can have more frequent check-ins with your doctor, which means catching issues before they become big problems. This leads to better health outcomes and less stress for everyone involved.
Specific Patient Benefits
- Remote consultations: See your doctor without leaving home.
- Convenience: Schedule appointments that fit your life.
- Reduced travel: Save time and money on trips to the clinic.
- Better chronic disease management: More frequent check-ins.
- Mental health services: Access care when you need it most.
Personalized care and patient satisfaction are where telemedicine in DPC truly shines. Since you’re not rushed through appointments, your doctor can take the time to get to know you and your health needs. This leads to more personalized treatment plans and a stronger doctor-patient relationship. Plus, happier patients mean better adherence to treatment plans and overall improved health. Now that’s a win-win!
Challenges and Solutions in Implementing Telemedicine in Direct Primary Care
Implementing telemedicine in Direct Primary Care (DPC) isn’t easy. One major challenge is the technological barrier. Many patients and providers may not have access to reliable internet or telehealth devices. Then, there are regulatory and reimbursement issues. Telemedicine policies vary by state, and navigating these can be tricky. Plus, integrating telemedicine into existing healthcare frameworks requires significant effort and resources.
Practical Solutions
- Invest in technology infrastructure: Ensure providers and patients access the necessary devices and reliable internet.
- Navigate regulatory frameworks: Stay informed about state-specific telemedicine policies and seek resources to comply with them.
- Provide training: Offer sessions to help everyone get comfortable with the new technology.
- Use secure communication platforms: Ensure these platforms comply with healthcare regulations to protect patient information.
- Collaborate with tech experts: Work with technology specialists to integrate telemedicine into your practice smoothly.
Overcoming these challenges can have a considerable impact on underserved populations. Together, telemedicine and DPC provide low-cost, convenient healthcare options, especially for those in rural or underserved areas. This means more people can access quality care without the usual barriers. The result? Reduced healthcare disparities and a healthier community overall.
Technology Requirements for Telemedicine in Direct Primary Care
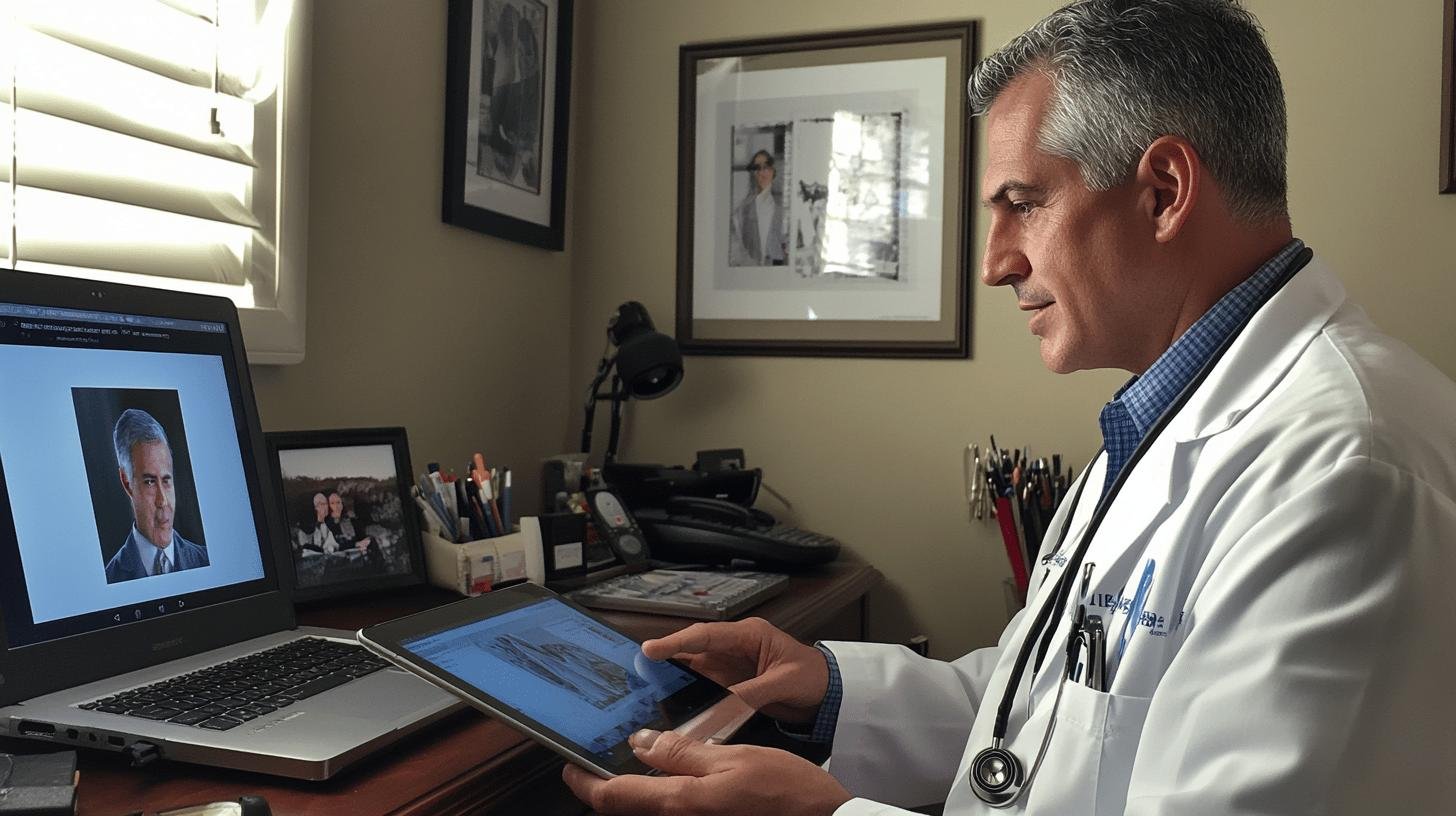
You need the right tech to make telemedicine work smoothly in Direct Primary Care (DPC). At its core, telemedicine relies on telecommunications technology. For secure consultations, you’ll need video conferencing tools, reliable phone lines, and online platforms. Think of it as a virtual clinic where patients can connect with their doctors without leaving their homes.
Secure communication platforms and electronic health records (EHR) systems are crucial for efficient telemedicine services. They ensure that patient data is protected and easily accessible. Imagine having all your health records at your fingertips while chatting with your doctor on a secure video call. This setup keeps your information safe and ensures your doctor has all the info they need to provide top-notch care.
Specific devices and internet requirements are the final pieces of the puzzle. Patients and providers need reliable internet connections to avoid those annoying “Can you hear me now?” moments. Plus, having suitable telemedicine devices like tablets, smartphones, or computers with webcams is essential. These devices allow thorough consultations, from discussing symptoms to showing visible health concerns.
| Technology | Importance |
| —————————– | ——————————————————— |
| Video Conferencing Tools | Enables face-to-face consultations |
| Secure Communication Platforms| Protects patient data and ensures privacy |
| Electronic Health Records (EHR)| Provides easy access to patient medical history |
| Reliable Internet Connection | Ensures smooth and uninterrupted communication |
Regulatory Considerations for Telemedicine in Direct Primary Care
Integrating telemedicine into Direct Primary Care (DPC) has its fair share of regulatory challenges. One of the biggest hurdles is that telemedicine policies vary widely from state to state. What works in one state may not be applicable in another. For example, some states have stringent requirements for telehealth consultations. This includes the need for an initial in-person visit before any virtual care can be provided. These varying regulations can make it difficult for DPC practices to implement a consistent telemedicine strategy across different locations. Additionally, there are often specific licensing requirements for healthcare providers who wish to offer telemedicine services, further complicating the landscape.
Reimbursement policies also play a significant role in DPC’s adoption of telemedicine. Unlike traditional healthcare models, where insurance companies often dictate reimbursement rates and procedures, DPC practices typically operate on a subscription basis. However, when telemedicine services are involved, understanding the nuances of reimbursement becomes crucial. For instance, some states have laws that mandate private insurers to cover telemedicine services at the same rate as in-person visits, while others do not. This variation can impact the financial viability of telemedicine services and requires DPC practices to stay well-informed about the latest telehealth regulations.
Success Stories and Case Studies of Telemedicine in Direct Primary Care

Patients rave about their experiences with Direct Primary Care (DPC) and telemedicine. The combo of convenience, affordability, and quality care makes it a hit, especially for folks in rural areas or those with mobility issues. Imagine not having to drive hours to see your doctor. Instead, you get personalized healthcare right from your living room. This setup boosts patient satisfaction, leading to better adherence to treatment plans and overall well-being.
Take, for instance, a DPC practice in a rural town where telemedicine was a game-changer. Patients who previously missed appointments due to long travel times could now consult their doctors via video calls. This led to improved health outcomes and higher patient satisfaction scores. Another example involves a patient with a chronic illness who needed frequent check-ins. Telemedicine allowed for more regular monitoring, resulting in better-managed symptoms and a higher quality of life. These real-life examples show that integrating telemedicine into DPC doesn’t just make healthcare more accessible; it makes it more effective.
Key Takeaways:
- Increased patient satisfaction: Convenient care right from home.
- Improved health outcomes: Regular check-ins lead to better management.
- Accessibility: Beneficial for rural areas and those with mobility issues.
Final Words
Navigating telemedicine in Direct Primary Care is like striking healthcare gold. We started by detailing how DPC and telemedicine work, then dove into the perks like accessibility and cost savings.
We also tackled the challenges, solutions, and tech you need to get rolling.
Why does it matter? Telemedicine in Direct Primary Care means more convenient, accessible, and personalized care. It’s a game-changer for healthcare.
So, are you ready to embrace the future of health with telemedicine in Direct Primary Care?
FAQ
Is telemedicine considered direct patient care?
Telemedicine allows patients to receive healthcare services digitally, so it can be considered direct patient care when it’s used to diagnose and manage patient health.
What is the difference between telemedicine and virtual primary care?
Telemedicine involves digital consultations for various healthcare needs. Virtual primary care is a more comprehensive model, focusing on ongoing patient health management through regular digital interactions with a primary care provider.
What are the benefits of telemedicine in primary care?
The benefits of telemedicine in primary care include increased access to healthcare, reduced travel needs, convenience of care from home, and better management of chronic conditions.
Which of the following situations is not considered part of telemedicine?
Any in-person consultation or healthcare service requiring physical presence is not considered telemedicine. Telemedicine strictly involves remote, digital healthcare services.