TL;DR:
- Financial Barriers: 60% of Americans struggle with high healthcare costs; U.S. healthcare spending was $4.5 trillion in 2022. Key issues include high deductibles, costly premiums, and unexpected bills.
- Geographic/Transportation: 67% face transportation issues; rural areas lack providers, leading to longer waits and missed appointments.
- Socio-Cultural: 1 in 5 U.S. households speaks a non-English language, which creates communication barriers. Cultural beliefs and health literacy affect care access.
- Systemic/Policy: Complex administrative processes delay care; inequitable policies create access inequalities.
- Solutions: Telemedicine, mobile health units, and community health programs improve access and engagement. Culturally competent care and language assistance are essential.
Ever felt like healthcare is about as affordable as a golden unicorn? You’re not alone! Over 60% of Americans find healthcare costs to be a massive hurdle. Barriers when accessing healthcare. This article dives into these big financial roadblocks and what we can do about them. Let’s explore how we can make healthcare less of a financial nightmare and more like grabbing your favorite cup of coffee—easy and stress-free!
Financial Barriers to Accessing Healthcare
Financial barriers cause many American adults to delay or skip medical care. Over 60% of Americans say healthcare costs are a big issue. In 2022, the U.S. spent a staggering $4.5 trillion on healthcare! That’s a massive amount. Insurance gaps make it even harder for people to access preventive care or regular pediatric checkups.
What contributes to these costs? High out-of-pocket expenses constitute a significant problem, especially for the uninsured. It’s like a wallet that leaks money with every doctor visit. This financial strain often leads to missed appointments or untreated conditions, creating a vicious cycle.
Common financial barriers people face include:
- High Deductibles: You must pay a lot before insurance helps.
- Costly Premiums: Just having insurance can strain your budget.
- Out-of-Pocket Expenses: Co-pays and medication costs add up quickly.
- Limited Coverage: Not all plans cover every necessary service.
- Unexpected Medical Bills: Surprise bills can hit hard.
So, how can we overcome these financial challenges? Affordable healthcare solutions are essential. Programs offering sliding scale fees based on income or community health initiatives providing low-cost services are vital. Expanding insurance coverage can also help, ensuring more people receive care without financial hardship. It’s all about making healthcare accessible without financial stress.
Geographic and Transportation Barriers to Healthcare Access

Imagine living miles from the nearest clinic with no bus route nearby. Transportation issues affect 67% of Americans, especially in rural areas. In addition to the pandemic, with 18% of healthcare staff leaving, healthcare access has become challenging. Let’s explore these barriers.
Geographic Barriers
Why do rural areas struggle? A lack of healthcare providers is a major factor. Fewer doctors mean longer waits and farther trips for patients. It’s like searching for a needle in a haystack. This shortage worsened post-pandemic, with many healthcare workers exiting the field, leaving a skeletal staff to cover vast areas. It’s not ideal at all.
Transportation Barriers
Can’t get to the doctor? You’re in good company. Transportation issues hinder healthcare access. Without reliable transport, patients miss routine checkups and urgent care. It’s like trying to win a race with a flat tire! Those in rural areas often depend on friends or family for a ride or skip visits entirely, delaying treatments and worsening health conditions.
|Barrier Type|Impact|
|—|—|
|Geographic|Shortage of providers leads to long waits and travel|
|Transportation|Lack of reliable transport means missed appointments|
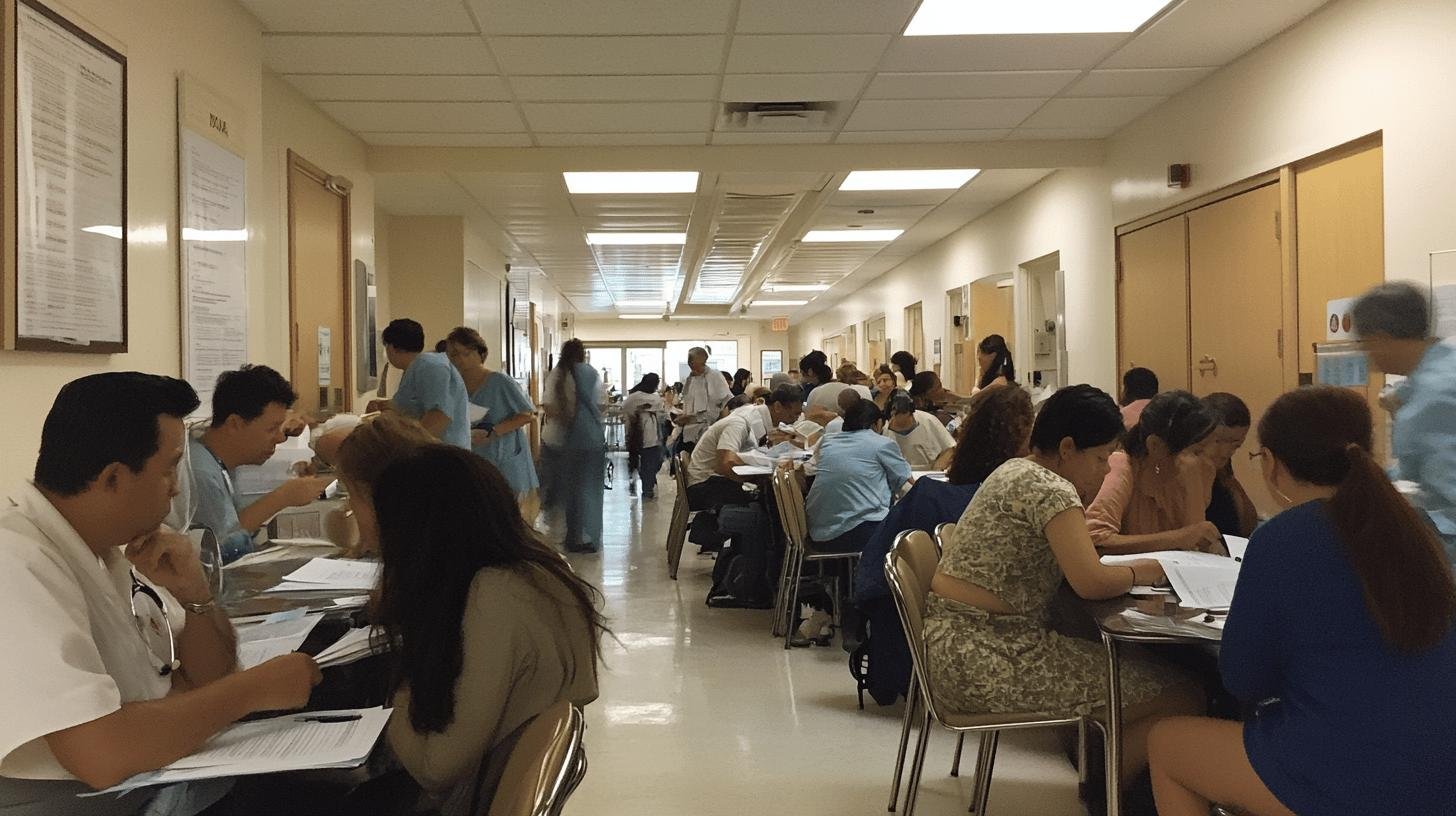
Socio-Cultural Barriers to Healthcare Access
Explaining a medical symptom to someone who doesn’t speak your language is like playing charades with your health. Language barriers are significant, with 1 in 5 U.S. households speaking a non-English language, causing misunderstandings or incorrect treatments. Cultural differences also play a role. Some avoid care due to beliefs not aligning with conventional medicine; past negative experiences can lead to hesitation.
Key socio-cultural barriers include:
- Language Differences: Miscommunication may result in wrong diagnoses.
- Cultural Beliefs: Some practices clash with Western medicine.
- Past Negative Experiences: Bad past interactions deter future care.
- Health Literacy: Not everyone understands medical jargon.
How do we tackle these barriers? Cultural competence and professional interpretation services are crucial. Culturally competent care respects different beliefs, improving patient comfort and trust. Access to professional interpreters helps bridge language gaps, ensuring patients and providers communicate effectively. These strategies create a more inclusive, effective healthcare environment for everyone.
Systemic and Policy Barriers to Healthcare Access
Let’s discuss the red tape in healthcare. Systemic barriers are like mazes, complicating access to care. Complex administrative processes can turn a simple doctor’s visit into a paperwork marathon—like solving a puzzle without all the pieces.
Systemic Barriers
Ever tried booking an appointment but faced mountains of forms? Complex administrative processes are a hurdle. Hospitals and clinics bogged down in regulations slow patient care, making it tough to get help. It’s like waiting in line for a ride at a park—minus the fun or treats at the end.
Policy Barriers
Policies can either open doors or slam them shut. When health equity is prioritized, it promotes fair access. Without focusing on diverse needs, policies create inequalities, leaving some out in the cold. It’s like having a key that doesn’t fit any lock.
|Barrier|Solution|
|—|—|
|Complex Administrative Processes|Streamline paperwork to speed up care|
|Inequitable Policies|Implement health equity initiatives for fair access|
Solutions to Overcoming Barriers in Healthcare Access
Facing healthcare barriers can feel like scaling a wall without gear, but modern solutions help! Telemedicine and patient engagement tech connect you with healthcare providers from home. Imagine resolving health questions via video call instead of waiting in a clinic. Mobile healthcare units offer essential services in hard-to-reach rural areas—a clinic on wheels!
Key healthcare access solutions include:
- Telemedicine: Virtual visits bring healthcare to you.
- Patient Engagement Tech: Apps and portals keep you informed.
- Mobile Health Units: Clinics on wheels reach remote areas.
- Community Health Programs: Local initiatives provide support.
- Culturally Competent Care: Services respect diverse needs.
- Language Assistance Services: Professional interpreters bridge communication gaps.
How effective are these solutions? Telemedicine thrived during the pandemic, offering safe, convenient consultations. It’s like having your doctor on speed dial! Mobile health units reach underserved communities, providing crucial services. Some neighborhoods see more preventive visits, cutting later emergency needs. It’s about bringing healthcare to people, ensuring everyone gets the care they deserve.
Community health programs also make a big impact. They offer culturally relevant services, boosting trust and participation. When people feel welcomed and understood, they’re more engaged in their healthcare—like finding a healthcare partner who speaks their language. These solutions don’t just break down barriers; they build bridges to better health for all.
Final Words
Tackling the barriers to accessing healthcare isn’t just a wish; it’s a necessity. We’ve looked at how financial, geographic, socio-cultural, and systemic hurdles can make getting care a real challenge. This tricky puzzle includes high costs, distance, language differences, and complex policies.
But hope shines through with innovative solutions like telemedicine and outreach programs, making healthcare more reachable. As we continue this journey to break down these barriers, embracing change is our best shot. Together, we can make healthcare a privilege and a reality for everyone.
FAQ
What are the barriers to accessing healthcare?
Accessing healthcare can be tricky due to financial issues, geography, transportation, and socio-cultural differences. High costs and lack of insurance keep many away, while remote locations and service shortages make trips tough. Language and cultural gaps also play a role.
Why is access to healthcare important?
Healthcare access matters because it boosts well-being and helps catch issues early. Health problems might worsen without it, leading to costly treatments or poor outcomes. It’s about keeping people healthy and detecting issues promptly.
What are the financial barriers to healthcare?
Financial barriers include high costs, lack of insurance, and inadequate coverage. These hurdles make people delay or skip care, impacting preventive measures and pediatric visits. Out-of-pocket charges can be hefty.
What are some examples of barriers to health?
Examples of health barriers include:
- Skyrocketing costs
- Lack of transport to providers
- Language differences
- Cultural myths about illnesses
These issues make getting care more challenging.
What is the healthcare access barriers model?
The model categorizes obstacles into several areas: financial, geographic, socio-cultural, and systemic. It helps identify where barriers are strongest, focusing on solutions to enhance access for everyone.
What factors affect access to healthcare?
Healthcare access hinges on factors like economic status, insurance type, geographic location, and cultural norms. Addressing costs, boosting provider availability, and fostering cultural understanding are necessary to overcome these.

