TL;DR:
- Autoimmune diseases, affecting 5-10% of the U.S. population (80% women), include lupus, rheumatoid arthritis, and multiple sclerosis.
- Symptoms may worsen during pregnancy, such as increased fatigue and joint pain.
- Risks include miscarriage and preeclampsia; specific risks per condition are outlined (e.g., APS: blood clots, SLE: preterm birth).
- Management strategies: achieve remission before conception, continue medication under medical guidance, and maintain regular check-ups.
- Autoimmune diseases impact pregnancy outcomes, causing risks like stillbirth and low birth weight.
- Postpartum symptoms may include fatigue and joint pain; ongoing follow-up care is crucial.
- Direct primary care offers personalized, affordable healthcare, enhancing monitoring and management during pregnancy.
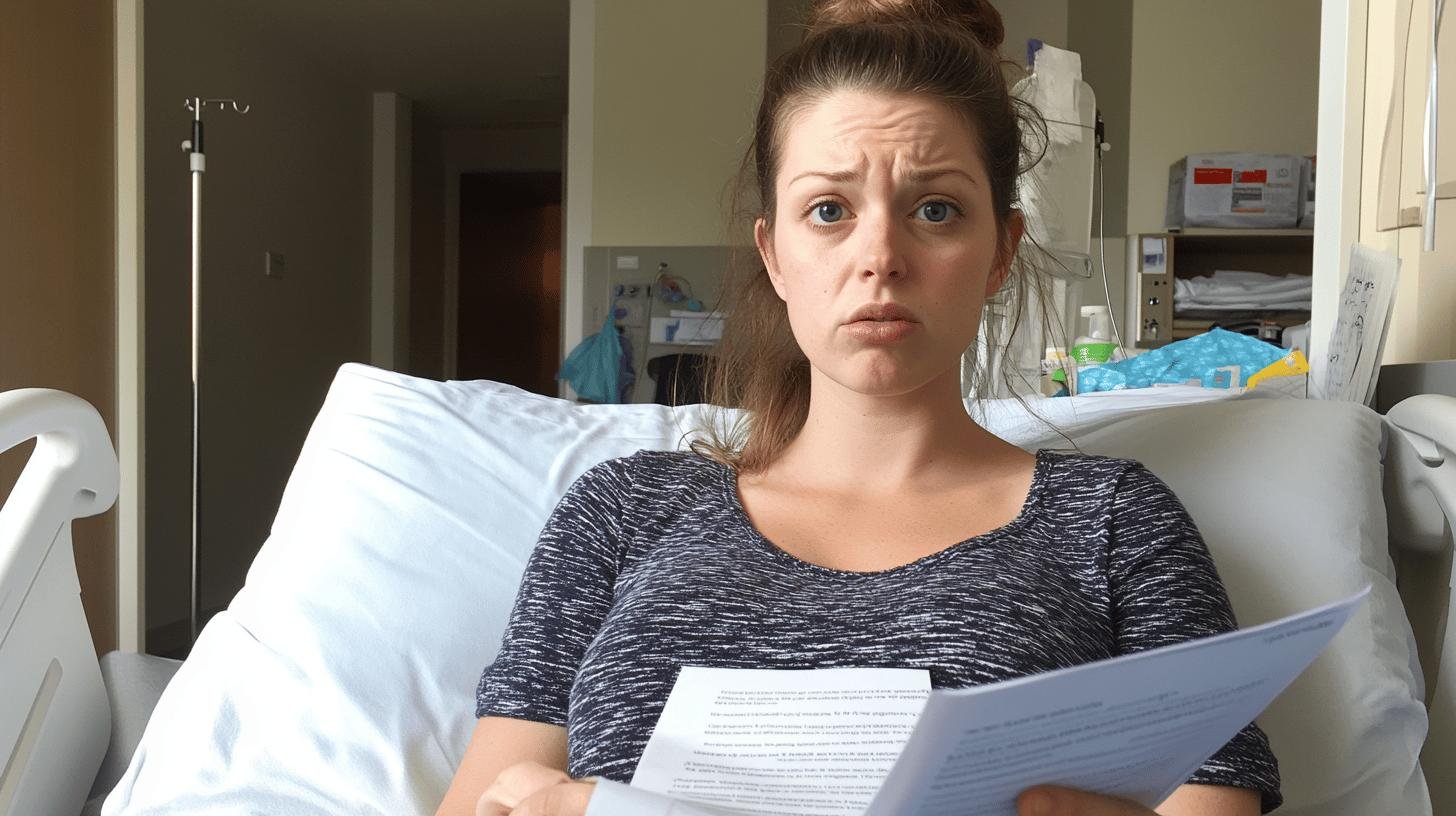
Ever wonder what happens when autoimmune diseases and pregnancy collide? With 80% of autoimmune warriors being women in their reproductive years, it’s a mix that’s more common than you’d think. As the body’s immune system mistakenly attacks healthy tissues, conditions like lupus or rheumatoid arthritis can shake up the pregnancy journey. Understanding the ins and outs of this complex relationship helps moms-to-be navigate a smoother ride. Ready to learn how these conditions can impact pregnancy and what you can do about it? Let’s dive in!
Understanding Autoimmune Diseases and Pregnancy
Autoimmune diseases occur when the immune system, meant to protect us, mistakenly attacks healthy tissues. Common examples include lupus, rheumatoid arthritis, and multiple sclerosis. You might be surprised to learn that these diseases affect 5-10% of the U.S. population. Even more striking is that 80% of those affected are women, often during their reproductive years. This creates unique challenges for women dealing with these conditions during pregnancy.
What about the symptoms? Autoimmune disorders cause a range of symptoms, such as fatigue, joint pain, and muscle weakness. During pregnancy, these might worsen or take unexpected turns. For example, fatigue can increase as pregnancy itself is tiring. Joint pain may feel more intense due to carrying extra weight. Monitoring symptoms closely and discussing any changes with healthcare providers is important.
Here’s a list of common autoimmune diseases affecting pregnant women:
- Lupus
- Rheumatoid Arthritis
- Multiple Sclerosis
- Sjögren’s Syndrome
- Systemic Sclerosis
Understanding these diseases is crucial for managing pregnancy effectively. By knowing what you’re facing, you can plan better for your care. Moms-to-be with autoimmune conditions need to be proactive and informed. Understanding how these conditions interact with pregnancy allows for tailored care plans, helping to keep both mom and baby healthy.
Risks of Autoimmune Diseases During Pregnancy

What are the risks of autoimmune diseases during pregnancy? Autoimmune conditions can complicate pregnancy, causing your immune system to attack healthy cells. This isn’t ideal when nurturing a baby. The main concerns include miscarriage and preeclampsia. Miscarriage happens when a pregnancy ends spontaneously before the 20th week. Preeclampsia involves high blood pressure appearing after the 20th week, leading to complications for both mother and baby.
Here’s a look into specific risks associated with different conditions:
| Condition | Associated Risk |
|———————|——————-|
| APS | Blood Clots, Miscarriage |
| SLE | Inflammation, Preterm Birth |
| Sjögren’s Syndrome | Miscarriage |
| Systemic Sclerosis | Intrauterine Growth Restriction |
How do these risks affect you and your baby? Conditions like APS and SLE can lead to inflammation and blood clots, posing dangers. Miscarriage and preterm birth bring emotional and physical challenges. Systemic sclerosis could restrict a baby’s growth. Teaming up with healthcare providers to manage these risks is vital, ensuring a healthy journey for you and your baby.
Managing Autoimmune Diseases During Pregnancy
Planning a baby with autoimmune diseases? Let’s discuss strategies! Achieving remission for six months before conception is ideal. This reduces complications during pregnancy. When symptoms are controlled, the body handles pregnancy demands better. Planning with healthcare providers assures you’re in optimal health before pregnancy.
Medication management is a major aspect. Continuing immunosuppressant medications often keep flare-ups in check. However, tailor this with medical guidance. Adjusting meds without expert consultation could cause harm, so maintain open communication with healthcare providers.
Management strategies to keep in mind include:
- Regular prenatal check-ups
- Medication adjustments
- Balanced diet and exercise
- Stress management techniques
Direct primary care can be invaluable for autoimmune management during pregnancy. It offers affordable, continuous care, free from typical insurance constraints. With personalized attention, you can focus on staying healthy. It’s like having a dedicated healthcare partner.
Autoimmune Diseases’ Impact on Pregnancy Outcomes
How do autoimmune diseases impact pregnancy outcomes? They can create multiple challenges. These conditions increase risks like stillbirth, preterm birth, and low birth weight. An unpredictable immune system may affect fetal development, leading to various health issues.
Let’s zoom in on specific conditions: Type 1 diabetes mellitus (T1DM) and inflammatory bowel disease (IBD). T1DM affects blood sugar levels, risking stillbirth and preterm birth. IBD is linked to gestational diabetes and can cause preterm birth. Inflammation and nutritional problems from IBD may hinder fetal growth, causing low birth weight. These show autoimmune diseases directly affect both mother and baby.
Improving these outcomes requires collaboration. Research is ongoing, but teamwork among healthcare providers makes a difference. Integrated care can reduce risks and lead to healthier pregnancies. The goal is to ensure the best for both mom and baby.
Postpartum Considerations for Autoimmune Diseases
Are you wondering what happens to autoimmune diseases postpartum? Let’s explain. Postpartum is the body’s recovery phase, which can trigger changes in autoimmune conditions. Postpartum thyroiditis involves thyroid inflammation, possibly swinging between overactive and underactive. Rheumatoid arthritis might worsen, causing joint pain and stiffness. Hormonal and immune changes heighten this risk.
Common postpartum symptoms to watch for include:
- Fatigue
- Joint pain
- Thyroid dysfunction
- Mood changes
Why is postpartum follow-up care crucial? Tracking these symptoms helps manage them and detect early flare-ups. Direct primary care excels here with continuous support sans insurance red tape. This ensures comprehensive, personalized care, helping you thrive postpartum.
Direct Primary Care for Autoimmune Diseases and Pregnancy

Why is a comprehensive care plan vital for managing autoimmune diseases during pregnancy? Coordination between you, prenatal providers, and specialists is key. Tailored care plans ensure needs are addressed, as autoimmune diseases are unpredictable and need monitoring and updates. Direct primary care fits in perfectly, offering continuous, affordable health management. It facilitates seamless communication, ensuring the best care during pregnancy.
The benefits of direct primary care include affordability and personalized attention. It bypasses insurance for predictable, manageable costs. This model provides longer appointments and direct provider access, akin to a healthcare concierge. Such personalized care improves health outcomes for you and your baby, making healthcare more accessible and boosting confidence throughout your pregnancy journey.
Final Words
Navigating pregnancy with autoimmune diseases can feel like juggling a dozen plates—with a couple on fire! We delved into the nitty-gritty of how these diseases affect pregnancy and what risks they may pose. But here’s the silver lining: understanding the challenge allows you to manage it effectively.
Taking proactive steps like pre-pregnancy planning and medication management can make a world of difference. Direct primary care steps in as a reliable partner, making healthcare more affordable and personalized. Your path to a healthy pregnancy and motherhood is paved with knowledge and the right support.
FAQ
Can pregnancy trigger autoimmune disease?
Pregnancy can influence the immune system, potentially triggering or exacerbating autoimmune diseases due to hormonal and immune changes.
How to treat autoimmune disease during pregnancy?
Treating autoimmune disease during pregnancy requires careful management, often involving immunosuppressants and lifestyle adjustments to prevent flare-ups while ensuring the baby’s safety.
What are common autoimmune disease symptoms in pregnancy?
Symptoms of autoimmune diseases during pregnancy may include fatigue, joint pain, and increased inflammation, and the symptoms vary by condition.
How do autoimmune diseases relate to pregnancy loss?
Autoimmune diseases like antiphospholipid syndrome can increase the risk of pregnancy complications, including miscarriage.
Can autoimmune diseases affect getting pregnant?
Autoimmune diseases can impact fertility, but many women with these conditions conceive successfully with appropriate medical support.
Can an autoimmune disease affect pregnancy?
Autoimmune diseases can complicate pregnancy by affecting the mother’s immune response, potentially causing issues like preterm birth or maternal health problems.
Are autoimmune diseases suppressed during pregnancy?
Sometimes, pregnancy can naturally suppress autoimmune symptoms, although this varies by individual and condition.
Can you have a successful pregnancy with positive ANA?
Yes, many women with a positive ANA have successful pregnancies, but close monitoring and management are important.
What are the most common autoimmune diseases after pregnancy?
Common postpartum autoimmune diseases include thyroiditis and rheumatoid arthritis, which may flare or develop after delivery.

