TL;DR:
- Terminal neurological diseases cause severe, irreversible nerve cell degeneration, leading to disability and death.
- Common diseases include:
- Amyotrophic Lateral Sclerosis (ALS): 2-5 years post-diagnosis.
- Huntington’s Disease: 10-30 years post-symptom onset.
- Advanced Alzheimer’s Disease: 4-8 years post-diagnosis.
- Progressive Supranuclear Palsy (PSP): 5-10 years post-onset.
- Multiple System Atrophy (MSA): 6-10 years from diagnosis.
- Palliative and hospice care focuses on symptom management and quality of life.
- Strategies: Pain relief, physical and speech therapy, nutritional support, and psychological guidance.
- Direct Primary Care offers streamlined, affordable care with benefits like unlimited visits and transparent pricing.
Ever wonder what neurological diseases are terminal or what makes them terminal? It’s a heavy topic, but understanding it can really shed some light on the challenges those affected face. Terminal neurological illnesses like ALS, Huntington’s disease, and advanced Alzheimer’s progressively shut down our nervous system, leading to major disabilities and, ultimately, death. These conditions aren’t just difficult to manage; they’re currently beyond the reach of medical solutions. We’ll dive into what defines these terminal diseases and why their progression is often irreversible. So, let’s gear up to understand how these harsh realities unfold.
Understanding Terminal Neurological Diseases
Terminal neurological diseases are severe, affecting the nervous system drastically. They cause progressive nerve cell degeneration, worsening over time with no cure available yet. This often results in severe disability and, eventually, death.
These diseases become terminal due to their relentless progression. Day by day, the nervous system deteriorates, causing muscle weakness, cognitive decline, and loss of motor function. It’s like watching a slow-motion disaster. Medical science still struggles to find a reversal solution.
Below are some common terminal neurological diseases:
- Amyotrophic Lateral Sclerosis (ALS)
- Huntington’s Disease
- Advanced Alzheimer’s Disease
- Progressive Supranuclear Palsy (PSP)
- Multiple System Atrophy (MSA)
The reason these disorders are considered terminal lies in the complexity of the nervous system. Once damaged, it can’t heal itself. Like untangling a tightly knotted string, these conditions slowly erode bodily functions, leaving fewer options over time. Although a harsh reality, understanding it helps in managing what lies ahead.
Symptoms and Prognosis of Terminal Neurological Diseases

Let’s delve into what happens when terminal neurological diseases take centre stage. Symptoms vary but often include muscle weakness, cognitive decline, and motor function loss. It’s like a gradual shutdown of body and mind, advancing through stages and presenting new challenges and limitations at each step.
Here’s a table for a clearer view:
| Disease | Symptoms | Prognosis |
|---|---|---|
| Amyotrophic Lateral Sclerosis (ALS) | Muscle weakness, trouble speaking, breathing issues | 2-5 years post-diagnosis |
| Huntington’s Disease | Uncontrolled movements, cognitive issues, psychiatric problems | 10-30 years post-symptom onset |
| Advanced Alzheimer’s Disease | Severe memory loss, disorientation, speech loss | 4-8 years post-diagnosis |
| Progressive Supranuclear Palsy (PSP) | Balance issues, eye movement problems, stiffness | 5-10 years post-onset |
| Multiple System Atrophy (MSA) | Motor control issues, autonomic dysfunction, stiffness | 6-10 years from diagnosis |
Predicting life expectancy can be complex, ranging from months to several years. It depends on the disease and individual health. Factors like progression speed, health conditions, and care access affect longevity with these conditions. Understanding these variations aids in planning and managing care.
Care Strategies and Palliative Care for Terminal Neurological Diseases
Palliative care provides comfort for those facing terminal neurological diseases. It focuses on symptom management and quality of life improvement rather than attempting disease reversal. The aim is to address both physical and emotional needs. Hospice care is crucial, offering specialized pain management and ensuring dignity and peace.
Symptom Management Strategies
Effective symptom management requires a thoughtful approach. Here are strategies that can help:
- Pain Relief: Use medications to ensure comfort.
- Physical Therapy: Helps maintain movement and reduce stiffness.
- Speech Therapy: Assists with communication and swallowing difficulties.
- Nutritional Support: Ensures proper nutrition if swallowing is hard.
- Psychological Support: Offers counseling for emotional well-being.
These strategies can ease the journey, maintaining a better quality of life.
End-of-Life Care Planning
Planning end-of-life care is sensitive but essential. Consider these steps:
- Advance Directives: Create legal documents for care preferences.
- Care Team Coordination: Align all healthcare providers.
- Family Discussions: Discuss wishes and expectations with loved ones.
- Financial Planning: Address costs for peace of mind.
- Legacy Projects: Encourage activities creating lasting memories, like scrapbooks or videos.
These steps ensure a smooth and meaningful end-of-life journey, honouring wishes and dignity.
Emotional and Practical Support for Patients and Families
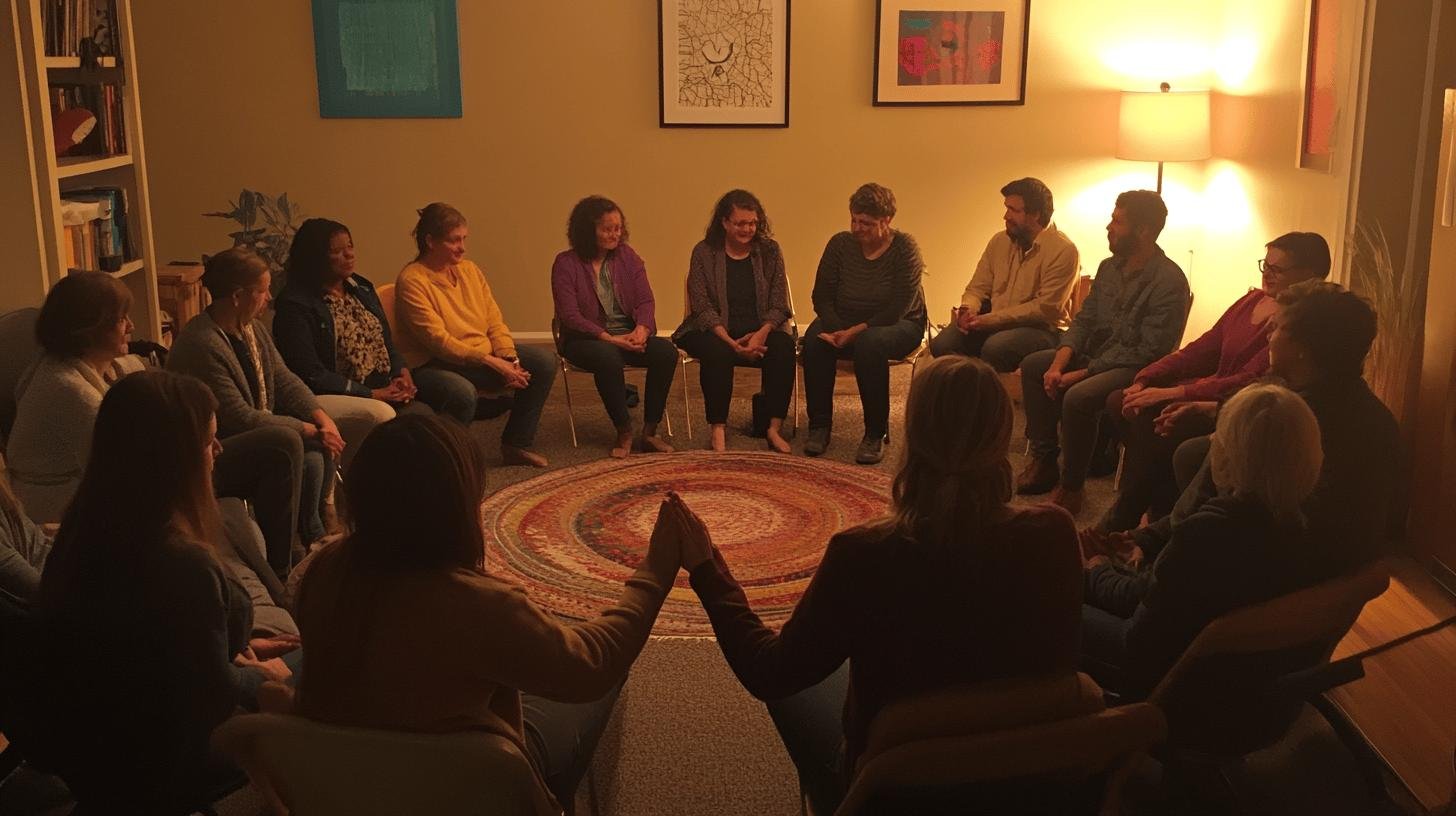
Facing terminal neurological diseases, emotional support becomes a lifeline for patients and families. These conditions are not just physically taxing but emotionally heavy. Coping strategies like counselling and support groups can lighten this burden. They provide a safe space to share feelings and experiences, making a world of difference.
- Support Groups: Connect with others in similar situations.
- Counselling Services: Professional guidance for emotional health.
- Hotlines: Immediate support in crises.
- Online Forums: Share and receive support anonymously.
- Mindfulness Apps: Tools for stress management.
Caregiver support is equally crucial, as this role can be overwhelming. Families should communicate openly, offering understanding and patience. Caregivers must seek help and take breaks to avoid burnout. After all, one cannot pour from an empty cup. These illnesses profoundly impact families, affecting dynamics and emotional well-being. Focusing on support and open communication helps families navigate this challenging journey together.
Direct Primary Care as an Affordable Option for Terminal Neurological Conditions
Are you wondering if there’s a simpler way to manage healthcare for terminal neurological conditions? Direct Primary Care (DPC) could be the solution. It bypasses insurance, providing smoother access to essential care. Patients pay a regular subscription fee for a range of primary care services without insurance hassles. This is ideal for conditions like ALS or advanced Alzheimer’s, where consistent care is crucial.
Here’s why direct primary care might be a game-changer:
- No Insurance Hassles: No waiting for approvals or claim issues.
- Transparent Pricing: Fixed monthly payments with no surprise bills.
- Unlimited Visits: No worries about co-pays for frequent check-ins.
- Personalized Care: Strong doctor relationships for tailored treatment.
- Convenient Communication: Contact your provider via calls, emails, or telemedicine.
Comprehensive care plans are possible with DPC. Doctors can focus on crafting plans that meet your unique needs without insurance distractions. This flexibility is vital for those navigating terminal neurological conditions, providing peace of mind.
Final Words
Navigating terminal neurological diseases like ALS and Huntington’s means facing brutal realities: progressive decline, severe symptoms, and, sadly, no current cure. Yet, focusing on care strategies can make an impact. From symptom management to comprehensive palliative care, we can do much to lift the quality of life.
Direct Primary Care emerges as a practical option, offering simplified, affordable access to needed care. While these disorders pose a tough battle, embracing holistic support and innovative care models can bring comfort and dignity to the journey. Words might fall short but hope and compassion don’t.
FAQ
Q: What are common terminal neurological diseases?
A: Terminal neurological diseases include ALS, Huntington’s disease, advanced Alzheimer’s, Parkinson’s disease, and multiple system atrophy. These illnesses lead to progressive degeneration and are often not reversible.
Q: What are the early symptoms of neurological disorders?
A: Early symptoms can include muscle weakness, memory issues, twitching, and difficulty walking. Catching these signs early helps in managing symptoms better.
Q: What are incurable neurological diseases?
A: Currently, incurable diseases are ALS and Huntington’s disease. Despite ongoing research, these conditions continue to challenge medical science with their irreversible nature.
Q: What neurological diseases are fatal?
A: Fatal neurological diseases include ALS, Huntington’s disease, and advanced Alzheimer’s. These conditions severely impact bodily functions, eventually leading to death.
Q: How do symptoms progress in terminal neurological diseases?
A: Symptoms typically worsen, starting with mild issues like muscle weakness and evolving into severe impairments such as loss of speech, motor skills, and cognitive decline.
Q: What is life expectancy in terminal neurological conditions?
A: Life expectancy varies; ALS may span 3-5 years, while advanced Alzheimer’s can last 8-10 years, though individual factors like overall health play a significant role.
Q: What are symptom management strategies for terminal neurological diseases?
A: Strategies include physical therapy, medications to manage pain and spasticity, nutritional support, respiratory care, and cognitive therapies to maintain mental function.
Q: How do you plan for end-of-life care?
A: Planning includes advance directives, discussing wishes with family, choosing hospice care, addressing financial aspects, and ensuring emotional support for everyone involved.
Q: What emotional support is available for patients and families?
A: Emotional support can include counselling, support groups, stress management techniques, spiritual guidance, and relaxation exercises to cope with the emotional toll.
Q: What are the advantages of direct primary care for terminal conditions?
A: Direct primary care offers personalized care, easy access to healthcare providers, transparent costs, longer doctor visits, and reduced administrative burdens for ongoing treatment.

